GreenMCMeds provides an advanced genomic solution by integrating pharmacogenomics testing (PGx) and therapeutic drug monitoring. This powerful combination improves clinical decisions, empowering physicians to create more precise and efficient treatment plans customized to individual patient needs.
With a steadfast dedication to scientific rigor and patient care, GreenMCMeds stands as a beacon of excellence in genetic services within Chicago. Drawing from over 30 years of combined clinical research experience, and bolstered by our cultural competence and unwavering commitment to diverse ethical standards, we adeptly cater to the varied needs of both patients and practitioners. Through this commitment, we uphold a gold standard of care.
Through our Strategic Holistic Ongoing Partnership (SHOP) Program, GreenMCMeds prioritizes community health by providing education and training to healthcare professionals and the broader community. Our data-driven, evidence-based approach ensures comprehensive service plans tailored to each patient, exemplifying our dedication to diverse, high-quality, personalized preventative care.
OUR COMPLETE Genetic Services
Personalized Medication Assessment
Our personalized medication metabolism assessment aims to enhance patient outcomes by addressing the shortcomings of trial-and-error medicine. Utilizing Pharmacogenomics (PGx) testing, we identify how individual genetic variations influence drug response, particularly in drug metabolism. The practitioner carefully reviews the detailed patient report, determining whether adjustments to medications are necessary or if current prescriptions should be maintained. Additionally, our PharmD hotline is readily available to address any questions or concerns from both patients and practitioners regarding their assessment report.
DISEASE CARRIER Screening
Our carrier screening analyzes 62 genes associated with 24 of the most prevalent and devastating hereditary diseases. Recommended for individuals in their reproductive stage (male or female, aged 18-45 years old), this test offers insight into the probability of passing one or more diseases from the panel down to their children. Moreover, it provides valuable genetic information irrespective of family planning intentions, benefiting individuals who are adopted or have an unknown family history.
Cancer Screening
Research indicates that up to 10% of cancers stem from inherited genetic factors, termed hereditary cancers. Genetic testing can assess an individual's susceptibility to these cancers by analyzing 31 genes associated with 8 different types of tumors, utilizing specific qualification criteria to determine risk levels. Offering this test empowers patients to proactively manage their health, potentially mitigating or even preventing the onset of cancer.
CARDIOVASCULAR DISEASE TESTING
Our non-invasive genetic test is designed to detect mutations associated with monogenic diseases of early atherosclerosis. The panel of genes analyzed influences plasma lipid levels (including total cholesterol, LDL, HDL, and triglycerides) as well as blood sugar. These targeted diseases significantly impact cardiovascular risk due to their early onset and poor prognosis without aggressive medical intervention. Patients meeting clinical criteria for familial hypercholesterolemia have a 60% to 80% chance of identifying the responsible mutation through our test. By detecting these mutations early, we can facilitate timely diagnosis and intervention to reduce cardiovascular risk.
Cancer Screening
Individuals at elevated risk for cancer have various options to mitigate their risk, including more frequent screenings, risk factor avoidance, lifestyle modifications, preventive medication (chemoprevention), and/or risk-reducing surgeries like mastectomy or oophorectomy. Our cancer screening panel encompasses tests for specific cancers such as breast, ovarian, colorectal, pancreatic, endometrial, gastric, skin, and prostate cancer. These screenings are personalized based on an individual's risk factors and medical history, aiding in the early detection of cancer when treatment is most effective. Early detection significantly improves the chances of successful treatment and survival.
DISEASE screening
Select the disease to get more detailed information.
SUGGESTED STEP-BY-STEP PROCESS TO
INCORPORATE TESTING IN YOUR OFFICE
Below is a suggested step-by-step process to seamlessly integrate testing into your office, thereby enhancing clinical judgment and improving patient quality of life:
- Pre-Screen Patients: Begin by pre-screening patients to identify those who meet the criteria for testing. This could involve reviewing medical records, discussing relevant family history, and considering other risk factors.
- Educate Patients: Have trained staff members explain the purpose and benefits of the test to eligible patients. Ensure patients understand the procedure and obtain their informed consent before proceeding.
- Sample Collection: Collect a sample from the patient's mouth using the provided swab. Make sure the collection process is performed correctly to ensure sample integrity.
- Documentation: Before shipping the sample, gather necessary documentation, including a copy of the patient's ID and insurance card (front and back). This ensures proper identification and billing procedures.
- Shipping Procedure: Package the collected samples according to the provided protocol. Utilize the prepaid shipping packaging and label included in the packet, which typically contains the requisition/consent form, swab, shipping package, and label.
- Shipping Logistics: Arrange for the shipment of the samples using the provided shipping label and packaging. Follow the designated shipping procedures to ensure samples reach the testing facility safely and efficiently.
- Cost Considerations: Emphasize to practitioners that all materials required for the testing process, including marketing materials and prepaid shipping packaging, are provided at no cost. Assure them that there are no start-up or ongoing expenses associated with providing these services.
By following this systematic approach, you can seamlessly integrate testing into your office workflow, providing patients with a more accurate, comprehensive, and effective treatment plan while minimizing administrative burdens and costs.
Disclaimer: GreenMCMeds provides health information solely for general informational and educational purposes to promote consumer health. This information should not be construed as medical advice or a replacement for proper medical care provided by a qualified practitioner. GreenMCMeds does not accept responsibility for any consequences resulting from the use of this information. It is the responsibility of the practitioner or medical professional to diagnose and administer appropriate care.
*GreenMCMeds is not involved in the cultivation or dispensing of cannabis, and we have no affiliations with dispensaries or cultivation sites.
FREQUENTLY ASKED QUESTIONS
Sample Reports
Gene Chart
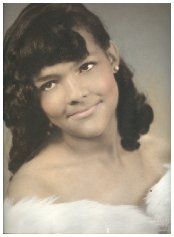
Our Inspiration
Mon Chéri remains a profound source of inspiration for us. Her courageous battle with brain cancer compelled us to reassess our approach to illness and disease, prescription drugs, and the critical significance of knowledge in both preventing and treating them. Additionally, her journey ignited our passion for plant science and its potential to heal not only individuals but also the world at large, driving us to explore innovative ways to harness the power of nature for holistic health and environmental sustainability.
Collaboration with CC Insurance
*GreenMCMeds is not involved in the cultivation or dispensing of cannabis, and we have no affiliations with dispensaries or cultivation sites.
© 2025 All Rights Reserved | GreenMCMeds

